Factors Affecting Personal Hearing Protector (PHP) Use Among Industrial Workers: Development and Validation of the Questionnaire
Main Article Content
Keywords
Personal hearing protectors, Industrial workers, Noise exposure, Questionnaire Development
Abstract
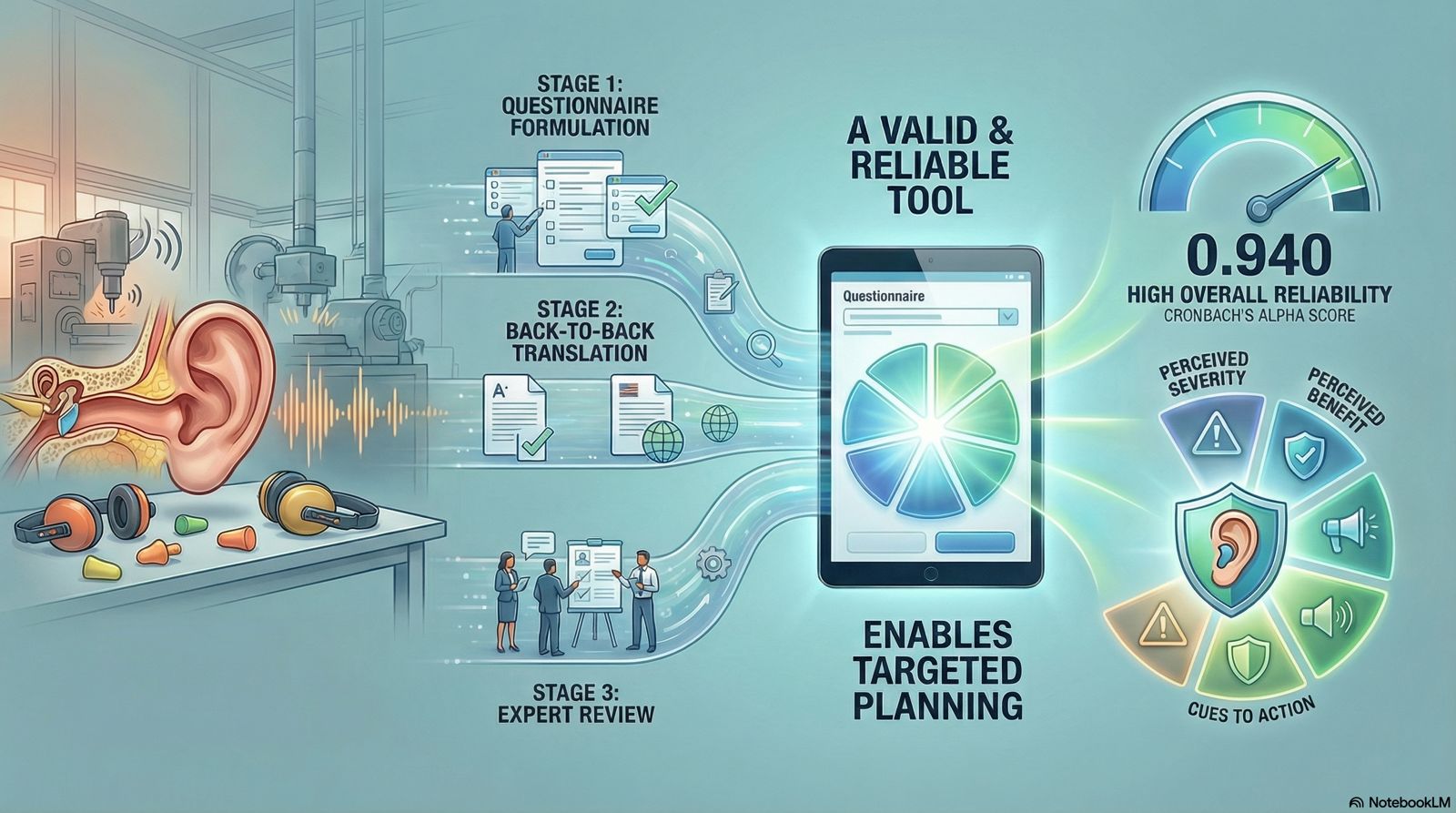
Personal hearing protectors (PHPs) used by industrial workers have already been a preferred measure in various industrial sectors that have issues with excessive noise exposure. Although personal hearing protectors (PHPs) are widely provided across industrial workplaces, actual worker compliance with their consistent and correct use remains notably low. Therefore, this study aimed to develop a valid measure to evaluate factors affecting PHP use among industrial workers in Malaysia. A questionnaire was developed on the factors affecting PHP use among industrial workers in Malaysia. The questionnaire comprised several items and was created using a systematic, thorough process consisting of three stages: (i) formulating items, (ii) translating them back-to-back, and (iii) subjecting them to expert content assessment by six (6) panels of experts. The questionnaire constructs and items were evaluated for content validity and reliability. The content validity score for each item was considered satisfactory. The Cronbach’s alpha was 0.940, indicating high overall internal consistency. The domain coefficients were as follows: interpersonal influence, 0.899; perceived severity, 0.902; perceived benefit, 0.868; perceived barrier, 0.893; perceived self-efficacy, 0.879; cues to action, 0.815; and use of PHP, 0.840. The domain coefficients demonstrated good to high internal consistency, ranging from 0.815 (cues to action) to 0.902 (perceived severity). This study shows that the questionnaire on factors affecting PHP use among industrial workers is valid and well-structured. Therefore, this study provides a valid and reliable tool for assessing factors influencing PHP use, which can inform the planning of targeted noise management programs.
Downloads
References
[2] S. N. S. Mamat, F. Naim, and F. Naim, “Noise exposure and perceived hearing symptoms of metal fabrication workers in heating, ventilating and air conditioning manufacturing industry,” Malaysian Journal of Medicine and Health Sciences, vol. 16, no. 12, pp. 135–143, 2020.
[3] H. Y. Kee, N. S. Fauzan and W. Mirta “Psychological impact of noise exposure among machine and non- machine operators in construction industry Psychological impact of noise exposure among machine and non-machine operators in construction industry,” IOP Conf. Ser. Mater. Sci. Eng., vol. 702, no. 012055, pp. 1–7, 2019, doi: 10.1088/1757-899X/702/1/012055.
[4] N. Tahir, S. M. Aljunid, and J. H. Hashim, “Occupational noise exposure in manufacturing industries in Malaysia,” BMC Public Health, vol. 14, no. S1, p. 2458, 2014, doi: 10.1186/1471-2458-14-s1-o17.
[5] Department of Statistics Malaysia, “National Occupational Accident and Disease Statistics 2021,” 2022.
[6] DOSH, “Occupational Diseases and Poisoning Statistic,” pp. 2016–2017, 2018.
[7] NIOSH, “National Institute for Occupational Safety and Health. Criteria for a Recommended Standard; Occupational Noise Exposure,” 1998.
[8] P. Campo et al., “Impact of noise or styrene exposure on the kinetics of presbycusis,” Hear. Res., vol. 280, no. 1–2, pp. 122–132, 2011, doi: 10.1016/j.heares.2011.04.016.
[9] G. A. Gates, P. Schmid, S. G. Kujawa, B. H. Nam, and R. D’Agostino, “Longitudinal threshold changes in older men with audiometric notches,” Hear. Res., vol. 141, no. 1–2, pp. 220–228, 2000, doi: 10.1016/S0378-5955(99)00223-3.
[10] DOSH, “Industry Code of Practice for Management of Occupational Noise Exposure and Hearing Conservation 2019,” Ind. Code Pract., 2019, [Online]. Available: dosh.gov.my/index.php/legislation/codes-of-practice/industrial-hygiene/3286-industry-code-of-practice-for-management-of-occupational-noise-exposure-and-hearing-conservation-2019/file.
[11] S. Ammar, A. Daud, A. F. Ismail, and A. Razali, “Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia,” Appl. Sci., vol. 12, no. 5, 2022, doi: 10.3390/app12052497.
[12] CDC. “Provide Hearing Protection,” The National Institute for Occupational Safety and Health, 2023. https://www.cdc.gov/niosh/topics/noise/preventoccunoise/provide.html#print (accessed Mar. 17, 2024).
[13] A. F. Ismail, A. Daud, Z. Ismail, and B. Abdullah, “Noise-induced hearing loss among quarry workers in a north-eastern state of Malaysia: A study on knowledge, attitude and practice,” Oman Med. J., vol. 28, no. 5, pp. 331–336, 2013, doi: 10.5001/omj.2013.96.
[14] Z. Haron et al., “Noise exposure among machine operators on construction sites in South Johor, Malaysia,” Adv. Mater. Res., vol. 838–841, pp. 2507–2512, 2014, doi: 10.4028/www.scientific.net/AMR.838-841.2507.
[15] C. S. Sam, W.Y., Anita, A.R., Hayati, K.S., Haslinda, A. and Lim, “Shift Work As a Predictor of Hearing Protection Devices Use Among Manufacturing Workers in Selangor, Malaysia,” Int. J. Public Heal. Clin. Sci., vol. 3, no. 2, pp. 2289–7577, 2016.
[16] A. Odu Ndep, J. Ebere Okeke, B. Nsa Ekpenyong, and N. C. Osuchukwu, “Using the Health Belief Model to Describe Factors Influencing Factory Workers’ Workplace Safety Practices in Nnewi, Anambra State, Nigeria,” Int. J. Innov. Sci. Res. Technol., vol. 5, no. 1, 2020, [Online]. Available: www.ijisrt.com.
[17] R. M. Rus, A. Daud, K. I. Musa, and L. Naing, “Knowledge, Attitude and Practice of Sawmill Workers Toward Noise-Induced Hearing Loss in Kota Bharu, Kelantan.,” Malays. J. Med. Sci., vol. 15, no. 4, p. 28, 2008.
[18] N. A. Ishak, N. S. Fauzan, and M. Widia, “Correlation Between Noise-Related Risk Perception, Knowledge and the Use of Hearing Protection Device: A Case Study Among Landfill Workers,” AIP Conf. Proc., vol. 2682, no. February, 2023, doi: 10.1063/5.0114277.
[19] R. R. Akbar-Khanzadeh F, Bisesi MS, “Comfort of personal protective equipment,” Appl Erg., vol. 26, no. 3, pp. 195–198, 1995, doi: https://doi.org/10.1016/0003-6870(95)00017-7.
[20] N. S. Fauzan, S. A. Mohd Zuki, E. H. Sukadarin, and M. Widia, “Preliminary study on the investigation of individual and organizational factors with the use of personal hearing protector (PHP) among industrial workers,” AIP Conf. Proc., vol. 3023, no. 1, pp. 1–9, 2024, doi: 10.1063/5.0189961.
[21] N. S. Fauzan, E. H. Sukadarin, M. Widia, I. Irianto, and I. Ghazali, “A Systematic Literature Review of the Factors Influencing Hearing Protection Device Usage among Industrial Workers,” Int. J. Environ. Res. Public Health, vol. 20, no. 4, 2023, doi: 10.3390/ijerph20042934.
[22] A. Wahab and M. Hamidi, “COVID-19 pandemic and the changing views of mobility: the case of Nepal–Malaysia migration corridor,” Comp. Migr. Stud., vol. 10, no. 1, pp. 1–19, 2022, doi: 10.1186/s40878-022-00320-1.
[23] L. Hwok-Aun and K. Y. Leng, “Counting Migrant Workers in Malaysia: A Needlessly Persisting Conundrum,” ISEAS Perspect., vol. 25, no. 1, pp. 1–11, 2018, [Online]. Available: https://www.iseas.edu.sg/images/pdf/ISEAS_Perspective_2018_25@50.pdf.
[24] R. Ismail, “Impact of foreign workers on labor productivity: Analysis of firm level data,” Int. J. Product. Qual. Manag., vol. 16, no. 1, pp. 36–53, 2015, doi: 10.1504/IJPQM.2015.070191.
[25] J. Shankar, D. Lai, S. P. Chen, T. C. Turin, S. Joseph, and E. Mi, “Highly Educated Immigrant Workers’ Perspectives of Occupational Health and Safety and Work Conditions That Challenge Work Safety,” Int. J. Environ. Res. Public Health, vol. 19, no. 14, 2022, doi: 10.3390/ijerph19148757.
[26] DOSH, Occupational Safety and Health (Noise Exposure) Regulations 2019. Putrajaya, Malaysia: Department of Occupational Safety and Health Malaysia, 2019.
[27] I. P. Nyarubeli, A. M. Tungu, S. Pallesen, B. E. Moen, and S. H. D. Mamuya, “Development and initial validation of questionnaire on predictors for the use of hearing protection devices among noise exposed manufacturing workers in Tanzania: A methodological study,” Front. Public Heal., vol. 11, 2023, doi: 10.3389/fpubh.2023.1102343.
[28] R. Neitzel, H. Meischke, W. E. Daniell, M. Trabeau, S. Somers, and N. S. Seixas, “Development and pilot test of hearing conservation training for construction workers,” American Journal of Industrial Medicine, vol. 51, pp. 120–129, 2008, doi: 10.1002/ajim.20531.
[29] G. H. Saunders, M. T. Frederick, S. Silverman, and M. Papesh, “Application of the health belief model: Development of the hearing beliefs questionnaire (HBQ) and its associations with hearing health behaviors,” Int. J. Audiol., vol. 52, no. 8, pp. 558–567, 2013, doi: 10.3109/14992027.2013.791030.
[30] N. Tantranont, K. & Codchanak, “Predictors of Hearing Protection Use Among Industrial Workers,” Workplace Health Saf., pp. 1–7, 2017, doi: 10.1177/2165079917693019.
[31] O. S. Hong, S. L. Lusk, and D. L. Ronis, “Ethnic differences in predictors of hearing protection behavior between Black and White workers.,” Res. Theory Nurs. Pract., vol. 19, no. 1, pp. 63–76, 2005, doi: 10.1891/rtnp.19.1.63.66339.
[32] O. Doutres, J. Terroir, C. Jolly, C. Gauvin, L. Martin, and A. Negrini, “Toward a Holistic Model Explaining Hearing Protection Device Use among Workers,” Int. J. Environ. Res. Public Health, vol. 19, no. 9, 2022, doi: 10.3390/ijerph19095578.
[33] O. Hong, D. L. Chin, and D. L. Ronis, “Predictors of Hearing Protection Behavior Among Firefighters in the United States,” Int. J. Behav. Med., vol. 20, pp. 121–130, 2013, doi: 10.1007/s12529-011-9207-0.
[34] D. L. Ronis, O. Hong, and S. L. Lusk, “Comparison of the Original and Revised Structures of the Health Promotion Model in Predicting Construction Workers ’ Use of Hearing Protection,” pp. 3–17, 2006, doi: 10.1002/nur.
[35] M. A. Pender, N. J. Murdaugh, and C. L. Parsons, Health Promotion in Nursing Practice, 7th ed. Norwalk, CT: Appleton & Lange, 2015.
[36] I. M. Rosenstock, “Historical Origins of the Health Belief Model,” Heal. Educ. Behav., vol. 2, no. 4, pp. 328–335, 1974, doi: 10.1177/109019817400200403.
[37] E. Taban, M. Yazdani Aval, O. Ahmadi, M. Miri, M. Fereidan, M. Rostami Aghdam Shendi, “Study of Personal Hearing Protection Devices Usage in Kashan Carpet Industry Workers,” Heal. Scope, vol. 5, no. 4, 2016, doi: 10.17795/jhealthscope-35250.
[38] M. C. Mccullagh, T. Banerjee, J. J. Cohen, M. A. and Yang, “Effects of interventions on use of hearing protectors among farm operators : A randomized controlled trial Effects of interventions on use of hearing protectors among farm operators : A randomized controlled trial,” Int. J. Audiol., vol. 55, pp. 3–12, 2016, doi: 10.3109/14992027.2015.1122239.
[39] A. Bockstael, L. De Bruyne, B. Vinck, and D. Botteldooren, “Hearing protection in industry : Companies ’ policy and workers ’ perception,” Int. J. Ind. Ergon., vol. 43, no. 6, pp. 512–517, 2013, doi: 10.1016/j.ergon.2012.08.009.
[40] K. Feder, D. Michaud, J. Mcnamee, E. Fitzpatrick, H. Davies, and T. Leroux, “Prevalence of Hazardous Occupational Noise Exposure , Hearing Loss , and Hearing Protection Usage Among a Representative Sample of Working Canadians,” JOEM, vol. 59, no. 1, pp. 92–113, 2017, doi: 10.1097/JOM.0000000000000920.
[41] O. Bolarinwa, “Principles and methods of validity and reliability testing of questionnaires used in social and health science researches,” Niger. Postgrad. Med. J., vol. 22, no. 4, p. 195, 2015, doi: 10.4103/1117-1936.173959.
[42] S. Tsang, C. F. Royse, and A. S. Terkawi, “Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine,” Saudi J. Anaesth., vol. 11, no. 5, pp. S80–S89, 2017, doi: 10.4103/sja. SJA_203_17.
[43] D. Kishore, Kamal; Jaswal, Vidushi; Kulkarni, Vinay; De, “Practical Guidelines to Develop and Evaluate a Questionnaire,” Indian Dermatol. Online J., vol. 12, no. 2, pp. 266–275, 2021, doi: 10.4103/idoj. IDOJ_674_20.
[44] V. Zamanzadeh, A. Ghahramanian, M. Rassouli, A. Abbaszadeh, H. Alavi-Majd, and A.-R. Nikanfar, “Design and Implementation Content Validity Study: Development of an instrument for measuring Patient-Centered Communication,” J. Caring Sci., vol. 4, no. 2, pp. 165–178, 2015, doi: 10.15171/jcs.2015.017.
[45] J. Yamada, B. Stevens, S. Sidani, J. Watt-Watson, N. De Silva, “Content validity of a process evaluation checklist to measure intervention implementation fidelity of the EPIC intervention,” Worldviews Evidence-Based Nurs., vol. 7, no. 3, pp. 158–164, 2010, doi: 10.1111/j.1741-6787.2010.00182.x.
[46] G. Toma, T. C. Guetterman, T. Yaqub, N. Talaat, and M. D. Fetters, “A systematic approach for accurate translation of instruments: Experience with translating the Connor–Davidson Resilience Scale into Arabic,” Methodol. Innov., vol. 10, no. 3, 2017, doi: 10.1177/2059799117741406.
[47] P. S. Cooper, D. R., & Schindler, Business Research Methods (11th ed.). New York: McGraw-Hill, 2011.
[48] M. A. Memon, H. Ting, T. Ramayah, F. Chuah, and J. H. Cheah, “A review of the methodological misconceptions and guidelines related to the application of structural equation modeling: A malaysian scenario,” J. Appl. Struct. Equ. Model., vol. 1, no. 1, pp. i–xiii, 2017, doi: 10.47263/jasem.1(1)01.
[49] C. H. Lawshe, “A quantitative approach to content validity,” Personnel Psychology, vol. 28, no. 4, pp. 563–575, 1975, doi: 10.1111/j.1744-6570.1975.tb01393.x.
[50] G. O. Boateng, T. B. Neilands, E. A. Frongillo, H. R. Melgar-Quiñonez, and S. L. Young, “Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer,” Front. Public Heal., vol. 6, no. June, pp. 1–18, 2018, doi: 10.3389/fpubh.2018.00149.
[51] M. S. B. Yusoff, “ABC of Content Validation and Content Validity Index Calculation,” Educ. Med. J., vol. 11, no. 2, pp. 49–54, 2019, doi: 10.21315/eimj2019.11.2.6.
[52] D. F. Polit and C. T. Beck, “Is the CVI an acceptable indicator of content validity? Appraisal and recommendations,” Research in Nursing & Health, vol. 30, no. 4, pp. 459–467, 2007, doi: 10.1002/nur.20199.
[53] A. A. Zulkeflee, N. Faisol, and F. Ismail, “Factors Influencing Foreign Workers’ Unwillingness to Practise Safety in The Malaysian Construction Sites,” Asian J. Res. Bus. Manag., vol. 4, no. 1, pp. 248–257, 2022, doi: 10.55057/ajrbm.2022.4.1.21.
[54] P. Thepaksorn, W. Siriwong, R. L. Neitzel, R. Somrongthong, and T. Techasrivichien, “Relationship Between Noise-Related Risk Perception, Knowledge, and the Use of Hearing Protection Devices Among Para Rubber Wood Sawmill Workers,” Saf. Health Work, vol. 9, no. 1, pp. 25–29, 2018, doi: 10.1016/j.shaw.2017.06.002.
[55] R. Reddy, D. Welch, S. Ameratunga, and P. Thorne, “Development of the hearing protection assessment (HPA-2) questionnaire,” Occup. Med. (Chic. Ill)., vol. 64, no. 3, pp. 198–205, 2014, doi: 10.1093/occmed/kqt178.